Clinical trials reach patients through primary care
Experts, administrations and industry agree that primary care is key to democratising access to drug trials and addressing the challenges facing the healthcare system.
Text: Anna Tañà | With the collaboration of Farmaindustria
Clinical research is at a turning point in Spain and, for the first time, primary care (PC), the level of care closest to the public, is at the centre of the debate. The ICAP Conference, an annual meeting promoted by Farmaindustria, brings together autonomous communities, researchers, professionals, patients and pharmaceutical companies to promote a single goal: for health centres to participate in a structured manner in drug research.
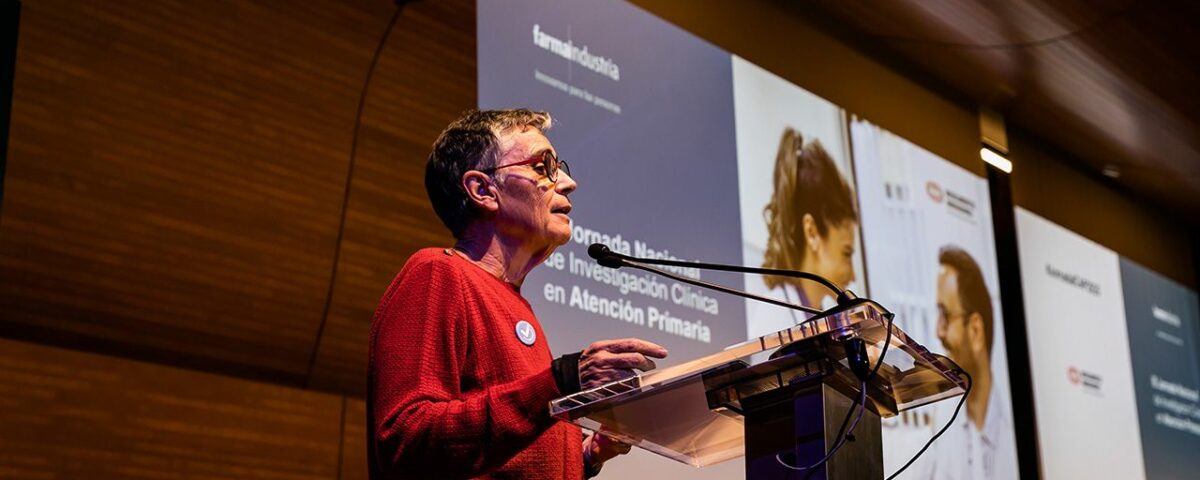
At the 3rd ICAP National Conference, held in Barcelona, health authorities, researchers and industry representatives agreed on a clear message: if Spain wants to consolidate its position as an international benchmark, clinical trials must move out of hospitals and into health centres, where patients are treated on a daily basis.
elperiodico.com
Leadership in trials, the challenge of proximity
The institutional welcome was given by Miguel González, from Farmaindustria, who recalled that clinical research is ‘one of the areas in which we can walk around the world with pride, setting an example for others’. He stressed that Spain is already ‘one of the world’s leading countries’ in clinical trials, but that the challenge now is to attract more studies and bring them closer to more patients. As he explained, the priority is for research to reach ‘the whole country’ and not be concentrated solely in large hospitals.
At the opening ceremony, the president of Farmaindustria, Fina Lladós, reinforced this vision with figures. In 2024, the innovative pharmaceutical industry exceeded €1.5 billion in R&D investment, and in 2023 alone it allocated €900 million to clinical trials (studies that evaluate new treatments before their approval), ‘of which nearly 80% are promoted by the industry’. ‘Spain is a country for research,’ she said, before arguing that innovation ‘must also reach health centres and not remain solely in hospitals’. For Lladós, primary care is ‘a real opportunity to transform the system and improve patients’ lives,’ which is why work is being done on stable research networks linked to health centres, such as the collaboration with the Generalitat’s CAIROS committee.

Elperiodico.com
The Minister of Health, Olga Pané, provided a historical perspective that helped to understand the changes experienced in primary care. She explained that decades ago, medical records were filed in folders that were ‘blue for men and pink for women,’ an anecdote that illustrates the lack of digitisation at the time. Today, however, Catalonia has 27 integrated reference centres that work with digital tools, artificial intelligence and new models of care. ‘Primary care makes more than 60 million contacts a year. It’s not just about retaining talent or generating knowledge: it’s about providing real solutions to real problems,’ she said.
Pané also highlighted the economic impact of research: ‘It produces knowledge, improves public services, boosts the economy and contributes to the country’s wealth.’ He pointed out that Spain ranks fifth in Europe and ninth worldwide in terms of the number of trials, and that companies choose the country ‘because of the quality of our studies.’ However, he warned that the healthcare system ‘will only be viable if primary care expands its scope, reaches people’s homes and solves problems where patients live.’ And he left a message that marked the day: without public-private collaboration, ‘it is impossible to generate the knowledge we need.’
The inaugural lecture by Dr Josep Basora, director of IDIAP Jordi Gol, gave an idea of the potential of this level. He explained that IDIAP has conducted 511 clinical trials between 1996 and 2024, most of them in phase III, i.e. the final stage in which the efficacy and safety of a drug is tested on large groups of patients. Basora highlighted that the institute is ‘the only institution that manages the entire value chain of clinical trials from and for primary care,’ from advising centres to authorisations and contracts.

elperiodico.com
Data, AI, and real-world evidence
He also highlighted the role of health databases such as SIDIAP, which compiles millions of anonymised medical records, and the European DARWIN project, designed by the European Medicines Agency to generate real-world evidence. Looking ahead to 2030, he anticipated trials that are ‘more patient-centred, more diverse and more inclusive’, supported by artificial intelligence, big data analysis and genomic tools that will enable increasingly personalised medicine. ‘Technology will be an essential support,’ he warned, ‘but it cannot replace the human factor. And that human factor is in primary care.’
The first round table provided an opportunity to learn about the progress made by the autonomous communities. Mariola Penadés, from the Valencian Community, explained the creation of a ‘one-stop shop’ to manage clinical trials and standardise procedures. Galo Peralta, from Cantabria, detailed the construction of a cohort of 50,000 volunteers (20% of the regional population) who provide valuable data through questionnaires, activity bracelets and biological samples.
From La Rioja, Manuel Ignacio Ruiz de Ocenda highlighted that the 20 health centres share electronic medical records with hospitals, which facilitates research and communication between levels of care. The Balearic Islands’ perspective was provided by Oana Bulilete, who emphasised networking and institutional support to promote studies in primary care.
Carmen de Vicente represented Andalusia, explaining that this autonomous community has a consolidated R&D strategy in health that includes specific calls for primary care and mixed dedication models (50% care and 50% research). ‘Primary care is where health is cooked up,’ she stated emphatically.

elperiodico.com
Training and less bureaucracy
The second round table focused on training, presented as a key element for the development of clinical research in primary care. Arantxa Sancho, from Farmaindustria, announced that the ICAP training course will be launched in 2026 with the participation of companies such as Sanofi, Novartis, MSD, AstraZeneca and the Spanish Medicines Agency. Vicente Pallarés, from SEMERGEN, argued that ‘there is a desire to research’, although many projects are left half-finished due to a lack of support. Mercedes Luz, from AstraZeneca, stated that training ‘is critical infrastructure for both professionals and patients’. Tatiana Massarrah, from Gregorio Marañón Hospital, reminded us that the priority must be the patient: “Bureaucracy slows things down. The pandemic has taught us that we can be more agile without losing rigour.‘ And Javier Malpesa, from Novartis, summarised the current keys to a trial: ’enthusiasm, collaborative work and fluid communication between all stakeholders.”
The 2026 Action Plan, presented by Sandra Sistiaga of GSK, detailed the eight strategic lines derived from the ICAP Guide: spreading the culture of research, certifying health centres, showing where research is carried out in primary care, promoting regional networks, promoting decentralised trials (studies that allow part of the follow-up to be carried out outside the hospital), strengthening public-private collaboration and simplifying processes and contracts. The spokesperson for the Platform of Patient Organisations, Paula Echeverría, recalled that ‘the main barrier to participating in trials is that many patients do not know they exist,’ and called for tailored information and feedback on results.
The conference ended with a shared message: Spain is already a leader in clinical trials, but now it also wants to be a leader in proximity, equity and citizen participation. Clinical research has begun to take root in primary care and, for the first time, the system seems determined to make it a stable pillar. The revolution, discreet but steady, is already underway.

elperiodico.com
Closing: collaboration and resilience of the system
The event closed with speeches by Javier Urzay, from Farmaindustria, and Manel del Castillo, president of CAIROS. Urzay emphasised the ambitious nature of the ICAP project and the need for primary care to participate so that Spain can continue to grow as a powerhouse in clinical research, recalling that ‘better care is always linked to better research’. Del Castillo explained that CAIROS was created to strengthen a healthcare system which, despite strengths such as high life expectancy, faces critical challenges: accelerated ageing, a shortage of professionals, an overload of care and a loss of confidence reflected in the increase in dual insurance. He advocated a profound transformation supported by new tools such as AI, new professional profiles and more agile management models, citing the Integra-Dependencia programme, which will reduce the assessment of dependency from more than a year to just a few months thanks to simplified circuits.
Del Castillo concluded that the only way to ensure the future of the public system is to move forward together, with a long-term vision and resilience in the face of change.